In all my reading about cancer biology, I have yet to tackle The Emperor of All Maladies, which is said to be the best book on the subject. Luckily, PBS and Ken Burns have delivered a three-part series based on Siddhartha Mukherjee's 2011 book. Here, I will do a short synopsis of Part Three, "Finding the Achilles Heel", which focuses on the development of cancer therapies.
The documentary begins with the story of Gleevec (covered beautifully in Jessica Wapner's The Philadelphia Chromosome), which was designed specifically to treat a type of chronic myelogenous leukemia (CML) that is caused by a swapping of two chromosomes to create the Philadelphia chromosome. The success of Gleevec led to great hope – could this be the first of many targeted therapeutics? Indeed, there have been some successes in targeted therapies; ALK inhibitors have shown some promise for the treatment of cancers that are characterized by the presence of an ALK gene rearrangement. However, on average, only four targeted therapy drugs are approved per year. These drugs are typically very expensive and are not very successful in terms of extending patients' lives.
The complexity of cancer has been a major obstacle in the development of successful therapeutics. When the human genome was completed in 2001, a new hypothesis arose: if we sequence common cancers and compare with normal cells, we could begin to understand exactly how they differ. In 2005, The Cancer Genome Atlas (TCGA) project began; this large-scale sequencing project aims to identify mutations in 25 different types of commonly occurring cancers. The first results, released in September 2008, confirmed cancer's complexity. Many cancers had multiple mutations in as many as 100 genes. However, there were some cancers that had only a few mutations or showed recurrent mutations, which were found in many different patients. These less complex cancers are the focus of future directions. As more and more cancer genomes are completed, researchers can start to identify patterns in the mutations that appear in cancers; such analyses may lead to the identification of driver mutations (i.e., mutations that are causally linked to oncogenesis) versus passenger mutations (i.e., mutations that are picked up along the way). Mukherjee points out how much drug companies have benefited from the information from basic research. He suggests that the current funding environment, where increased funding of clinical and translational studies comes at the expense of basic research, is not likely to promote these types of success stories in the future.
The shift in focus from cancer treatment to cancer prevention has generally been a useful approach. For example, smoking was once a major contributor to cancer, but anti-smoking campaigns starting in the late 1960's have successfully reduced the number of new lung cancer cases. Obesity is another major contributor, but solving this health problem has been less straightforward. Viruses like human papilloma virus (HPV) and hepatitis are also common causes for cancers; these viruses are now decreasing in incidence with vaccines for both viruses available. Approximately 40% of cancers are due to unknown causes. Epidemiology focuses on determining a causal link between cancers and environmental factors (e.g., pollution, occupation, cell phones), but the connections are often difficult to prove (as was discussed in Toms River.) Overall, the combination of prevention, early detection, and targeted therapies has decreased the cancer mortality rate 20% in the US over the last two decades.
For me, the most interesting part of the this episode was about cancer immunotherapy. Cellular immunotherapy takes immune cells from a patient's blood, activates these cells, and then gives them back to the patient; this approach boosts the immune system by enriching for T cells. Some researchers have suggested that the immune system is held back from attacking cancer because it is the patient's own cells. In 1992, the FDA approved a therapy using interleukin-2 (IL-2), a protein produced by white blood cells during the immune response. Increasing IL-2 leads to increased T cell response, making T cells more likely to recognize and attack cancer cells. After that initial success, there were few breakthroughs, but some recent developments have increased interest in the field. For example, in 2011 the FDA approved Yervoy (ipilimumab), which binds and blocks CTLA-4, a checkpoint protein that prevents T-cell activation to keep cells from attacking healthy tissue. Thus, when CTLA-4 is blocked, T cells can attack tumors. Both Yervoy and IL-2 treatment show long-lasting responses, but only in a small percentage of patients; serious side effects are also common. The newest weapon in the immunotherapy arsenal is an inhibitor of PD-1, called Opdivo (nivolumab). PD-1 is another checkpoint protein, which some cancers use to disable the T cells in the area surrounding the tumor. PD-1's specificity to cancer cells suggests that Opdivo could be more powerful and less toxic than existing therapies. Based on these exciting developments, this is likely an area to watch in the coming years.
--------------------------------------------
** You can read more about cancer immunotherapy in this feature in Nature, this Nature review by Ira Mellman, or the April 2015 special issue of Cancer Cell focused on immunotherapy in cancer.
The documentary begins with the story of Gleevec (covered beautifully in Jessica Wapner's The Philadelphia Chromosome), which was designed specifically to treat a type of chronic myelogenous leukemia (CML) that is caused by a swapping of two chromosomes to create the Philadelphia chromosome. The success of Gleevec led to great hope – could this be the first of many targeted therapeutics? Indeed, there have been some successes in targeted therapies; ALK inhibitors have shown some promise for the treatment of cancers that are characterized by the presence of an ALK gene rearrangement. However, on average, only four targeted therapy drugs are approved per year. These drugs are typically very expensive and are not very successful in terms of extending patients' lives.
The complexity of cancer has been a major obstacle in the development of successful therapeutics. When the human genome was completed in 2001, a new hypothesis arose: if we sequence common cancers and compare with normal cells, we could begin to understand exactly how they differ. In 2005, The Cancer Genome Atlas (TCGA) project began; this large-scale sequencing project aims to identify mutations in 25 different types of commonly occurring cancers. The first results, released in September 2008, confirmed cancer's complexity. Many cancers had multiple mutations in as many as 100 genes. However, there were some cancers that had only a few mutations or showed recurrent mutations, which were found in many different patients. These less complex cancers are the focus of future directions. As more and more cancer genomes are completed, researchers can start to identify patterns in the mutations that appear in cancers; such analyses may lead to the identification of driver mutations (i.e., mutations that are causally linked to oncogenesis) versus passenger mutations (i.e., mutations that are picked up along the way). Mukherjee points out how much drug companies have benefited from the information from basic research. He suggests that the current funding environment, where increased funding of clinical and translational studies comes at the expense of basic research, is not likely to promote these types of success stories in the future.
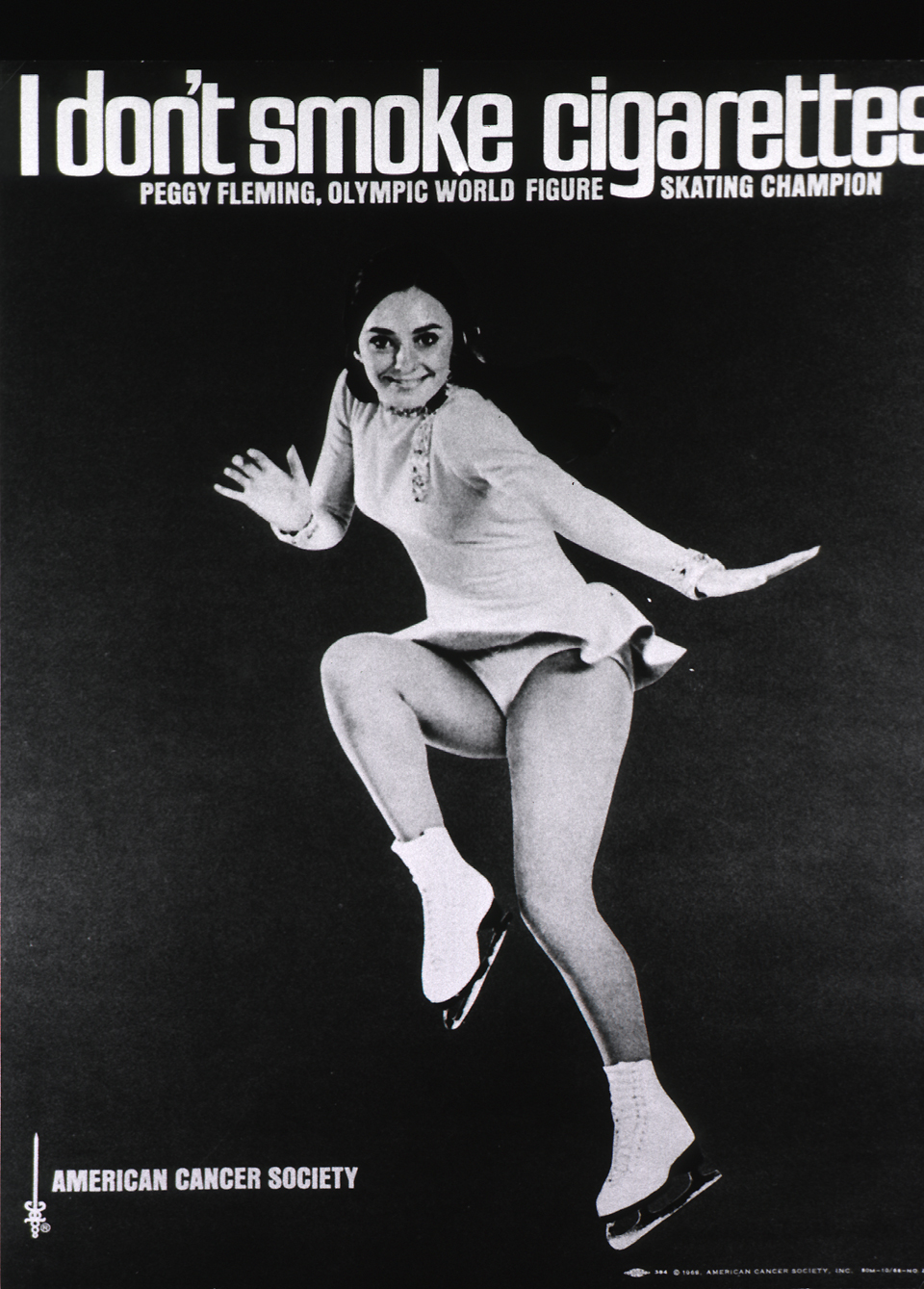 |
| ACS, anti-smoking ad 1968 |
For me, the most interesting part of the this episode was about cancer immunotherapy. Cellular immunotherapy takes immune cells from a patient's blood, activates these cells, and then gives them back to the patient; this approach boosts the immune system by enriching for T cells. Some researchers have suggested that the immune system is held back from attacking cancer because it is the patient's own cells. In 1992, the FDA approved a therapy using interleukin-2 (IL-2), a protein produced by white blood cells during the immune response. Increasing IL-2 leads to increased T cell response, making T cells more likely to recognize and attack cancer cells. After that initial success, there were few breakthroughs, but some recent developments have increased interest in the field. For example, in 2011 the FDA approved Yervoy (ipilimumab), which binds and blocks CTLA-4, a checkpoint protein that prevents T-cell activation to keep cells from attacking healthy tissue. Thus, when CTLA-4 is blocked, T cells can attack tumors. Both Yervoy and IL-2 treatment show long-lasting responses, but only in a small percentage of patients; serious side effects are also common. The newest weapon in the immunotherapy arsenal is an inhibitor of PD-1, called Opdivo (nivolumab). PD-1 is another checkpoint protein, which some cancers use to disable the T cells in the area surrounding the tumor. PD-1's specificity to cancer cells suggests that Opdivo could be more powerful and less toxic than existing therapies. Based on these exciting developments, this is likely an area to watch in the coming years.
--------------------------------------------
** You can read more about cancer immunotherapy in this feature in Nature, this Nature review by Ira Mellman, or the April 2015 special issue of Cancer Cell focused on immunotherapy in cancer.




